The Surprising Link Between Panic & Your Gut: The Mind-Body Connection
Interconnectedness of Panic & The Digestive System
Looking at symptoms or disorders in silos does a great disservice to you as a patient. Everything in the body is connected! The brain and digestive system (aka the gut) are no different. Disease can begin in the gut or be exacerbated there, both in creating gastrointestinal (GI) dysfunction, but also creating other system dysfunction. Dr. Deborah Bowers, a Functional Pharmacist and Wellness Coach, uses a whole-body approach when searching for the root cause of panic/anxiety.
What Is Leaky Gut? Does It Cause Panic?
For anyone who has ever experienced a flood of dread or what we call a panic attack, we know just how debilitating that can be, as well as how much that can keep someone stuck in a sympathetic, dominant nervous system mode. This mode can cause you to feel like you're in danger, like you need to run or hide from a bear that's chasing you.
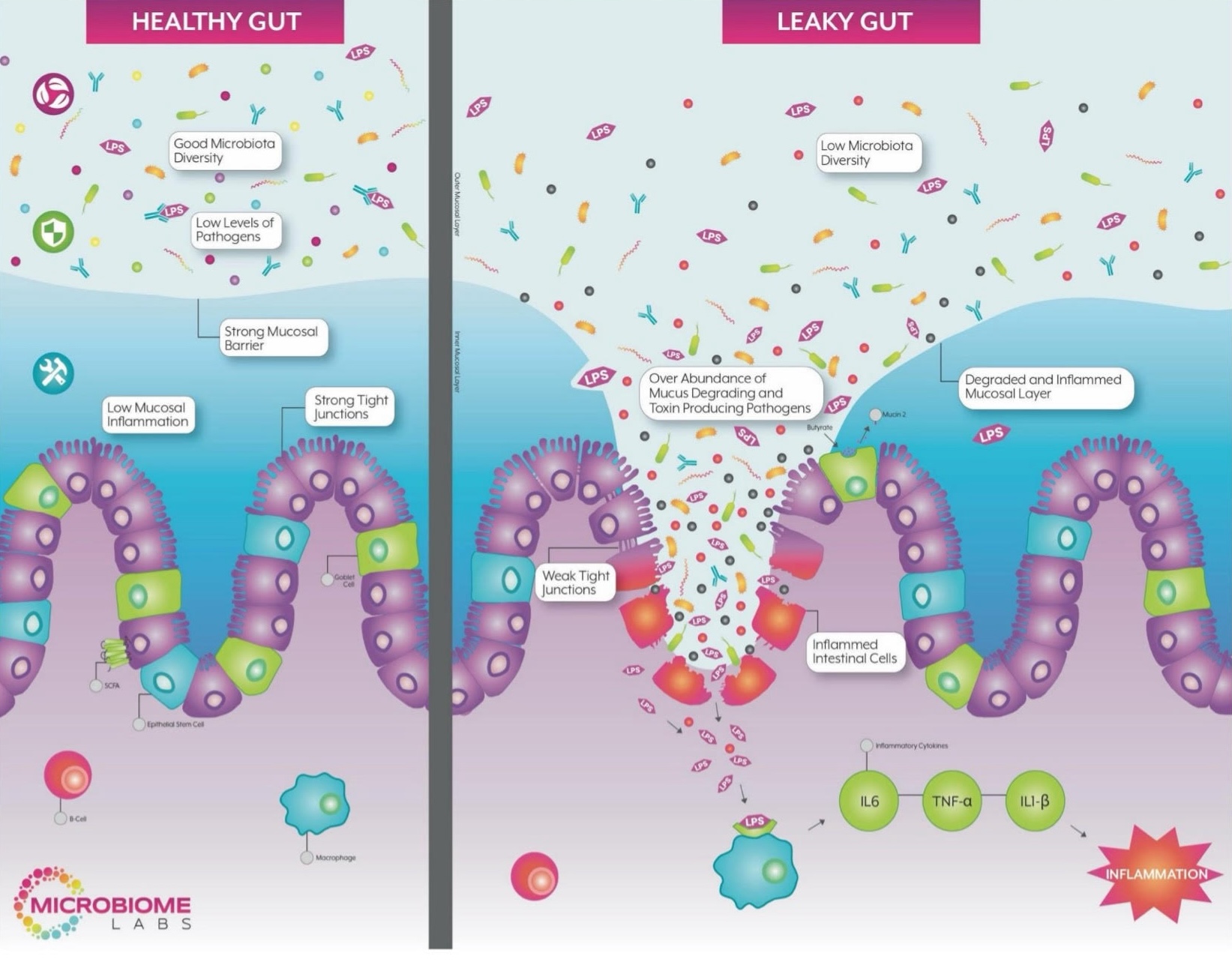
When there's a loss of barrier function in the intestines, we develop enhanced intestinal permeability, which is also called leaky gut. When that happens, what is at play in the gut doesn't stay there. It leaks out and causes inflammation and other problems.
The gut-brain axis allows the two systems to communicate or work together. Leaky gut affects the brain by attacking the blood-brain barrier, the barrier that's supposed to protect the brain. The blood-brain barrier isn't a bulletproof wall. It can be penetrated. This is one explanation of what causes panic attacks.
We know in particular that there's a rich, diverse microbiome and microbial debris in the gut that naturally occurs when we eat and digest food. The immune system is constantly surveying, and the GI tract is trying to excrete.
When we have a loss of barrier function, we are much more likely to give exposure of our immune system to this microbial debris, and in particular, pro inflammatory endotoxins, such as lipopolysaccharide (LPS's for short). This is going to be a stimulant of hypervigilance in the immune system and in the basement membrane of the intestines.
When there is a loss of barrier function, those inflammatory mediators, LPS's and other pro-inflammatory debris can gain systemic circulation. We know that key inflammatory mediators such as interleukin six (IL-6 for short), which is a hallmark of gut related inflammation. IL-6 build up can increase the permeability of the blood brain barrier, and also a buildup of histamine can increase blood brain barrier permeability.
Once that happens, the mood impacts of gut born imbalances where IL-6, in particular, can up regulate the behavior of our glutamate receptors (which is excitatory).
Leaky Gut, Neurotransmitters And Inflammation... Oh My!
Glutamate is the primary stimulatory neurotransmitter in the body, just like GABA is the primary inhibitory neurotransmitter in our nervous systems, and in our body overall.
When we get extra stimulation of the glutamate neurotransmission, it promotes a neurological and a cognitive hyper-vigilance that can easily lead to quite a bit of anxiety and vulnerability to panic.
What we see here is what happens in the gut doesn't stay in the gut. Inflammation is upregulated because of increased exposure to the immune system, especially in the gut, and gut associated lymphatic tissue. Then, circulation increases, which causes increased inflammation because LPS in the systemic body is not where it's supposed to be.
That impairment of the blood-brain barrier and downstream upregulation of receptors called NMDA receptors (they're glutamate receptors) and glutamate; all causes excitation.
We can further drive this by not having the correct nutritional co-factors needed to modulate the balance of GABA and glutamate. Magnesium is an example. This is why nutritional intake becomes important, in particular for the synthesis and neurotransmission of GABA. GABA is the primary inhibitory neurotransmitter in the body used to have good mood balance. This balance is important so you are not too hyper-stimulated, but also not too dull and numbed. We need to have good GABA- glutamate regulatory oversight and also flexibility in terms of allowing the body to move in and out of the various nervous system states, and neurotransmission balances that we need in order to navigate our world.
Inadequate magnesium, for example, often leads to inadequate GABA neurotransmission. This can lead even more to a GABA-glutamate imbalance, and a more glutamate dominant dynamic that can promote anxiety and also surges of panic.
To further complicate things, once you have those stress hormones from panic, magnesium (also not the only nutrient needed) degrades and gets rid of those excitatory neurotransmitters.
We can further connect some issues with food sensitivities that increase inflammation via the complement system. Additional inflammation comes from the gut and from dietary debris. This can also be another strong mediator of inflammation. This can have that same gut-brain axis impact on neurotransmission and modulation. There is also everything that we do lifestyle wise, in terms of stress, that is also going to further promote this process.

Histamine's Role In Panic & Anxiety
We can also connect histamine as a cause of panic.
Histamine promotes wakefulness all on its own. When histamine builds up, it overtly has that effect on the blood-brain barrier, increasing the stimulation of those glutamate receptors as well.
Another connection is as women age due to hormone fluctuations, we naturally don’t degrade histamine as well.
You can see how you can’t just look at one system. Everything is connected. We have to look at the body as a whole to see what is going on with a given individual, their circumstances, their needs, their environment, etc., to really help find healing.
You can start to see how something that we associate panic and anxiety as being a neurological symptom or challenge, a brain and central nervous system dynamic, can be easily mediated, not only by other below the neck, systemic dynamics, but also by what is happening in the gut. Specifically, when we lose barrier function, what's happening in the gut isn't staying there.
There is evidence internal to the gut itself, that our microbial byproducts have an impact on vagal stimulation, and so there's also a direct pathway by which what is happening in the gut and in our microbiome, is informing the brain and systemic nervous system, via the metabolites. (The vagus nerve connects the gut and brain. It's one of the longest nerves in the body.)
We've learned that various metabolites from our microbes impact the synthesis and neurotransmission of various neurotransmitters. In that way, our neurotransmitters can be a bit of a language by which our microbiome talks to our brain and talks to our central nervous system.
This is completely outside of the notion of loss of barrier function (called leaky gut). This is a way the gut is informing the brain and central nervous system about the status of our world on a regular, basis. It's a primary source of information going up through the vagus nerve that the brain then uses in making decisions about how it wants to regulate our entire torso, including other gut function, based on the information that it's gleaned from our entire life system.
We need to remember that a huge source of information coming into the brain is this huge transmission that is happening from the gut, informing the brain about the status of our world, the status of our microbiome, the status of our immune system and the status of our gut health.
Next Steps
I hope this is interesting and informative, as well as shows you a little peak into the work I do navigating all these puzzle pieces for a unique individual person and their circumstances with panic and anxiety.
If you'd like to discuss your health challenges with Dr. Deborah Bowers, Functional Pharmacist & Health Coach, schedule a complimentary discovery call here.
Related Posts
Why You Should Care What Goes In Your Mouth.
Have you ever heard of someone feeling better after modifying their diet? There are, in fact, several mechanisms of action to explain this claim. Click below to find out what those mechanisms are!

Dr. Deborah Bowers
822 B E Liberty St
York, SC 29745
(803)628-7934
© 2025 Dr. Deborah Bowers. All Rights Reserved.
Site Conceived By HealthProWebsite.com


